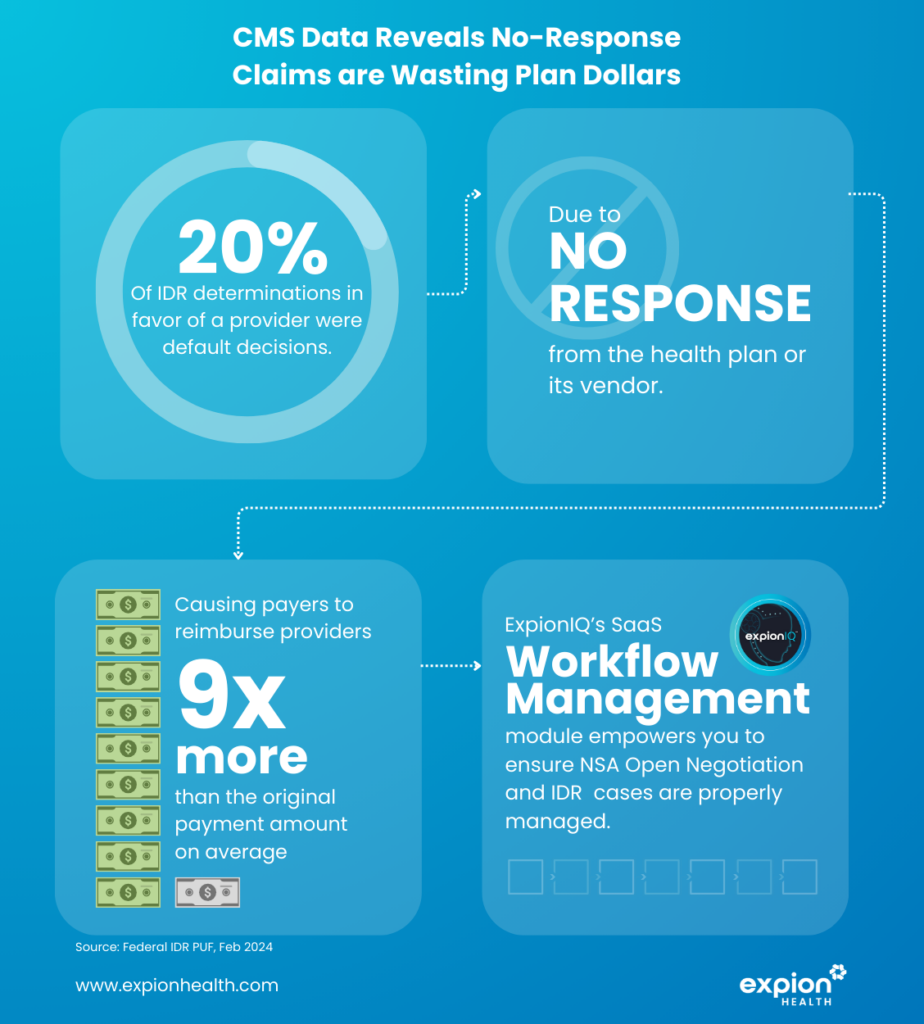
Expion Health’s analysis of the latest CMS report from February 2024, which sheds light on the Independent Dispute Resolution (IDR) process for No Surprises Act (NSA) cases. for the first half of 2023, uncovered a particularly interesting finding: plan dollars are being wasted on what we have termed “no-response” claims. These occur when health insurance plans or their vendors fail to respond to claims in IDR , leading to default decisions that overwhelmingly favor healthcare providers. This post delves into the implications of these findings and explores strategic solutions to mitigate these challenges.
The Findings: A Closer Look at IDR Cases
According to the CMS report, out of 178,000 IDR cases documented for Q1 and Q2 of last year, approximately 125,000 were ruled in favor of the provider. Out of that 125,000, around 20% (24k+), concluded in default decisions. This outcome primarily stems from the failure of health insurance plans or their vendors to respond to IDR submissions, resulting in providers being awarded payments averaging nine times the initial claim amount.
Understanding the Financial Implications
The financial implications of these default decisions are substantial. They not only inflate the costs for health insurance plans significantly but also highlights breakdowns in the dispute resolution process. This trend of no-response claims suggests a broader issue of inadequate workflow management within the industry, emphasizing the necessity for enhanced operational practices.
The Essential Role of Workflow Management
Effective workflow management is crucial in addressing the challenge of no-response IDR cases. It ensures timely and appropriate responses to IDR submissions, aligns with NSA and state balance billing regulations, and maintains operational efficiency. The absence of effective workflow management can lead to negative financial outcomes for health insurance payers, underscoring the importance of adopting comprehensive management solutions.
Introducing Expion Health’s Workflow Management Software
Expion Health provides a specialized Workflow Management software solution designed to tackle the challenges of the No Surprises Act IDR process outlined in the CMS report. Built on the ExpionIQ platform, our NSA Workflow Management tool is designed to assist health insurance plans in navigating NSA compliance and improving their dispute resolution processes. By adopting Expion Health’s software, organizations can prevent the unnecessary financial waste associated with no-response claims and enhance their operational effectiveness.
Explore how ExpoinIQ’s NSA Workflow Management software can streamline IDR case management, enabling compliance, response management, and better financial outcomes.