This month’s edition provides a focused review of newly approved and recently launched therapies. Expion Health monitors these developments closely to assess clinical relevance, therapeutic positioning, and potential implications for payers, providers, and patients.
KEYTRUDA QLEX

Indication
KEYTRUDA QLEX (pembrolizumab and berahyaluronidase alfa) is approved for the treatment of 38 indications, including melanoma, non–small cell lung cancer, malignant pleural mesothelioma, head and neck squamous cell carcinoma, urothelial carcinoma, microsatellite instability–high or mismatch repair–deficient cancers, colorectal cancer, gastric cancer, esophageal cancer, cervical cancer, hepatocellular carcinoma, biliary tract cancer, Merkel cell carcinoma, renal cell carcinoma, endometrial carcinoma, cutaneous squamous cell carcinoma, and triple-negative breast cancer.
Dosage and Administration
KEYTRUDA QLEX is administered as either a one-minute subcutaneous injection every three weeks or a two-minute injection every six weeks.
- One-minute injection: 395 mg of pembrolizumab and 4,800 units of berahyaluronidase alfa (2.4 mL total volume).
- Two-minute injection: 790 mg of pembrolizumab and 9,600 units of berahyaluronidase alfa (4.8 mL total volume). Injections should be administered subcutaneously in the thigh or abdomen by a healthcare provider.
Warnings and Precautions
KEYTRUDA QLEX may cause immune-mediated adverse reactions including pneumonitis, colitis, hepatitis, endocrinopathies, nephritis, and severe skin reactions, which may require corticosteroid treatment and therapy interruption. Other reported effects include hypophysitis, thyroid disorders, and diabetic ketoacidosis.
Mechanism of Action
KEYTRUDA QLEX combines pembrolizumab, a programmed death receptor-1 (PD-1)–blocking monoclonal antibody, with berahyaluronidase alfa, a recombinant human hyaluronidase PH20 enzyme. Pembrolizumab blocks the PD-1 receptor’s interaction with PD-L1 and PD-L2, reactivating T-cell–mediated immune responses against tumor cells. Berahyaluronidase alfa facilitates local dispersion and absorption of pembrolizumab, enabling subcutaneous administration without altering the drug’s anticancer activity.
Disease Background
Solid tumors are abnormal growths of tissue that form in solid organs such as the lung, breast, colon, and bladder. They are composed of heterogeneous cell populations including cancer cells, stem cells, connective-tissue cells, and immune cells, making them particularly challenging to treat.
Clinical Data
FDA approval was based on a multicenter, randomized, open-label Phase 3 trial evaluating subcutaneous KEYTRUDA QLEX versus intravenous KEYTRUDA in patients with treatment-naïve metastatic non–small cell lung cancer (NSCLC) without EGFR, ALK, or ROS1 genomic aberrations. Patients received either formulation every six weeks in combination with platinum-based chemotherapy. The confirmed objective response rate (ORR) was 45% with KEYTRUDA QLEX versus 42% with IV KEYTRUDA. No meaningful differences were observed in progression-free survival (PFS) or overall survival (OS). The most common adverse reactions (≥20%) were nausea, fatigue, and musculoskeletal pain.
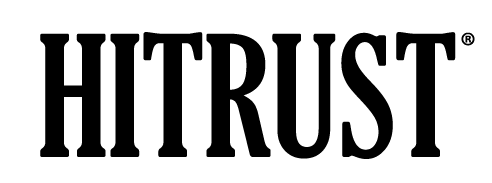
EYDENZELT
Indication
EYDENZELT (aflibercept-boav) is a biosimilar to EYLEA (aflibercept) approved by the FDA for the treatment of neovascular (wet) age-related macular degeneration (wAMD), macular edema following retinal vein occlusion (RVO), diabetic macular edema (DME), and diabetic retinopathy (DR).
Dosage and Administration
The standard dosing of EYDENZELT is 2 mg administered by intravitreal injection every four weeks. Dosing frequency may vary based on the treatment indication. EYDENZELT is available as a single-dose prefilled syringe or single-dose vial for ophthalmic use.
Warnings and Precautions
Serious ocular adverse events may occur following intravitreal injection, including endophthalmitis, retinal detachment, and retinal vasculitis with or without occlusion. Patients and caregivers should be advised to immediately report any signs or symptoms suggestive of infection, inflammation, or vision changes. Increases in intraocular pressure have been observed within 60 minutes post-injection. There is also a potential risk of arterial thromboembolic events following intravitreal use of VEGF inhibitors.
Mechanism of Action
Aflibercept is a vascular endothelial growth factor-A (VEGF-A) inhibitor that blocks the growth of new blood vessels and reduces vascular permeability in the eye. It binds to VEGF-A and placental growth factor (PIGF), preventing activation of VEGF receptors 1 and 2 (VEGFR-1 and VEGFR-2) on endothelial cells, which are responsible for neovascularization and vascular leakage.
Disease Background
- wAMD (wet age-related macular degeneration) is the leading cause of irreversible blindness and vision loss, characterized by abnormal blood vessel growth beneath the retina.
- RVO (retinal vein occlusion) occurs when a retinal vein becomes blocked, causing fluid buildup and macular swelling that distorts central vision.
- DME (diabetic macular edema) results from diabetes-related blood vessel damage, leading to fluid leakage and retinal swelling.
- DR (diabetic retinopathy) is caused by chronic damage to retinal blood vessels from elevated blood glucose levels.
Clinical Data
FDA approval was based on a randomized, double-masked, parallel-group, multicenter Phase 3 study comparing EYDENZELT with EYLEA in patients with DME. Results demonstrated equivalent efficacy, safety, pharmacokinetics, and immunogenicity between the two treatments. The most common adverse reactions (≥5%) included conjunctival hemorrhage, eye pain, cataract, vitreous detachment, vitreous floaters, and increased intraocular pressure.
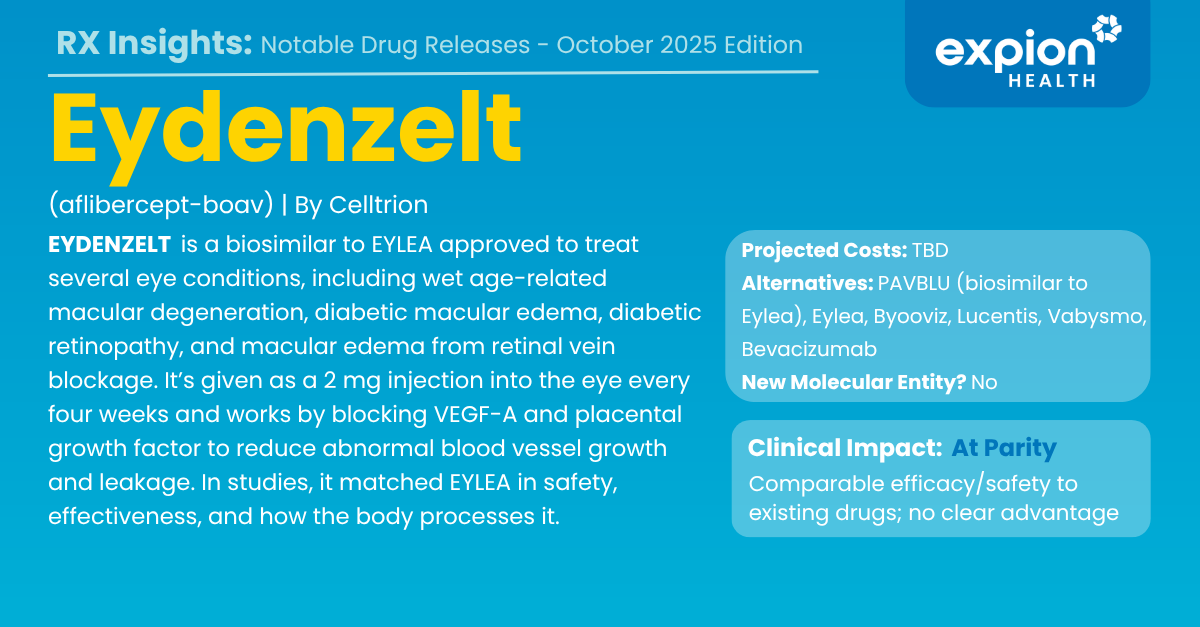
JASCAYD
Indication
JASCAYD (nerandomilast) is approved by the FDA for the treatment of idiopathic pulmonary fibrosis (IPF), a rare, progressive, and life-threatening lung disease with limited treatment options. It is the first new therapy approved for IPF in more than a decade.
Dosage and Administration
The recommended dose is 18 mg orally twice daily, approximately 12 hours apart, with or without food. JASCAYD is available as 9 mg and 18 mg tablets.
Warnings and Precautions
Common adverse reactions (≥5%) include diarrhea, COVID-19, upper respiratory tract infection, depression, decreased weight and appetite, nausea, fatigue, headache, vomiting, back pain, and dizziness. Patients should be monitored for mood changes, gastrointestinal tolerance, and signs of infection.
Mechanism of Action
Nerandomilast is a selective phosphodiesterase 4 (PDE4) inhibitor with at least nine-fold higher affinity for the PDE4B isoenzyme. PDE4 inhibition elevates intracellular cyclic adenosine monophosphate (cAMP), reducing the release of inflammatory cytokines and growth factors that drive fibrosis in IPF. These anti-fibrotic and immunomodulatory effects help slow disease progression.
Disease Background
Idiopathic pulmonary fibrosis causes thickening and stiffening of lung tissue surrounding the air sacs (alveoli), leading to permanent scarring and difficulty breathing. Symptoms typically include shortness of breath and chronic cough. Most patients are diagnosed between ages 60 and 70, with a median survival time of about five years following diagnosis.
Clinical Data
FDA approval was supported by two randomized, double-blind, placebo-controlled trials in adults with IPF. The primary endpoint measured change from baseline in Forced Vital Capacity (FVC)—the maximum amount of air exhaled after a deep breath. Patients treated with JASCAYD experienced significantly less decline in FVC compared to placebo, indicating slowed disease progression.
EPIOXA

Indication
EPIOXA is approved by the FDA for the treatment of keratoconus, a rare, progressive, and sight-threatening corneal disease that often goes undiagnosed and untreated. It is indicated for adult and pediatric patients aged 13 years and older. EPIOXA is the first and only epithelium-on, oxygen-enriched corneal collagen cross-linking treatment, offering an incision-free alternative to traditional procedures that require removal of the corneal epithelium.
Dosage and Administration
EPIOXA is administered in-office by an eye care professional.
- Step 1: Apply two drops of EPIOXA HD 0.239% riboflavin 5′-phosphate ophthalmic solution every 60 seconds for 4 minutes.
- Step 2: Apply two drops of EPIOXA 0.177% riboflavin 5′-phosphate ophthalmic solution every 30 seconds for 6 minutes.
Both formulations are supplied as single-dose glass syringes for topical application.
Warnings and Precautions
Corneal collagen cross-linking should be used with caution in patients with a history of herpetic keratitis, due to potential reactivation risk. The most common adverse reaction is conjunctival hyperemia. Other reactions (≤25% of treated eyes) include corneal opacity, photophobia, eye pain, irritation, dry eye, epithelial defect, eyelid edema, corneal striae, and anterior chamber flare.
Mechanism of Action
EPIOXA’s active ingredient, riboflavin 5′-phosphate, is activated by UV-A light during the procedure, creating new chemical bonds (“cross-links”) between collagen fibers in the cornea. This strengthens corneal tissue, stabilizes its shape, slows or halts disease progression, and helps preserve vision.
Disease Background
Keratoconus is a degenerative eye disorder characterized by thinning and weakening of the cornea, often progressing most rapidly in individuals under 30. If untreated, it can lead to severe visual impairment or blindness, and is a leading cause of corneal transplants in the U.S. About 90% of cases affect both eyes, and up to 20% of untreated patients eventually require transplantation. Conventional glasses or contact lenses only correct vision, not the underlying disease.
Clinical Data
FDA approval was supported by two prospective, randomized, multicenter, double-masked Phase 3 trials that achieved their pre-specified primary efficacy endpoints. Both studies demonstrated that EPIOXA provided significant improvement in corneal stability with a favorable safety and tolerability profile.
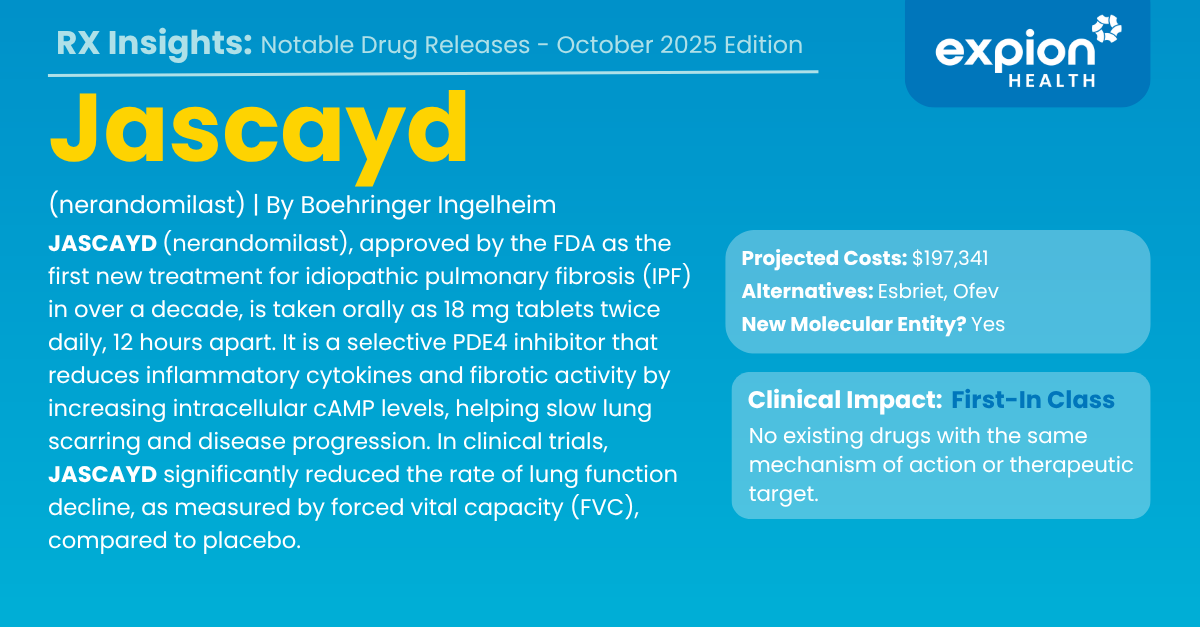
LYNKUET
Indication
LYNKUET (elinzanetant) is a non-hormonal prescription drug approved by the FDA for the treatment of moderate to severe vasomotor symptoms (VMS) associated with menopause.
Dosage and Administration
LYNKUET is supplied as a 60 mg capsule. The recommended dosage is 120 mg (two capsules) taken orally once daily at bedtime.
Warnings and Precautions
LYNKUET may cause somnolence, dizziness, vertigo, or presyncope. Patients should be advised to avoid driving or operating heavy machinery if these effects occur. Those with a history of seizures may be at increased risk. The most common adverse reactions (≥5%) include headache, fatigue, dizziness, abdominal pain, rash, diarrhea, and muscle spasms.
Mechanism of Action
Elinzanetant is a dual neurokinin 1 (NK1) and neurokinin 3 (NK3) receptor antagonist that acts on KNDy neurons within the hypothalamus. During menopause, declining estrogen levels lead to overactivation of these neurons, disrupting the body’s thermoregulatory center. By blocking NK1 and NK3 receptors, LYNKUET helps restore normal thermoregulation, reducing the frequency and severity of hot flashes and night sweats.
Disease Background
Vasomotor symptoms (VMS) are common menopausal symptoms caused by hormonal fluctuations and impaired temperature regulation. Up to 85% of women experience hot flashes or night sweats during menopause, which can significantly impact quality of life.
Clinical Data
FDA approval was based on the OASIS Phase 3 clinical trial program, which included the OASIS 1 and OASIS 2 studies. LYNKUET met primary endpoints demonstrating statistically significant reduction in the frequency and severity of vasomotor symptoms. Symptom relief began within seven days of therapy initiation, with over 80% of patients maintaining improvement by six months.